What Are Endosteal Implants? Learn More About the Dental Implant

Table of Contents
- What Are Endosteal Implants?
- How They Work
- Who Is a Candidate?
- The Endosteal Implant Procedure
- Recovery & Next Steps
Endosteal implants are a popular way for people to solve long-time poor teeth issues. An alternative to removable dentures or bridgework, the strong three-piece implants are made of titanium and can provide pain-free talking and chewing.
What Are Endosteal Implants?
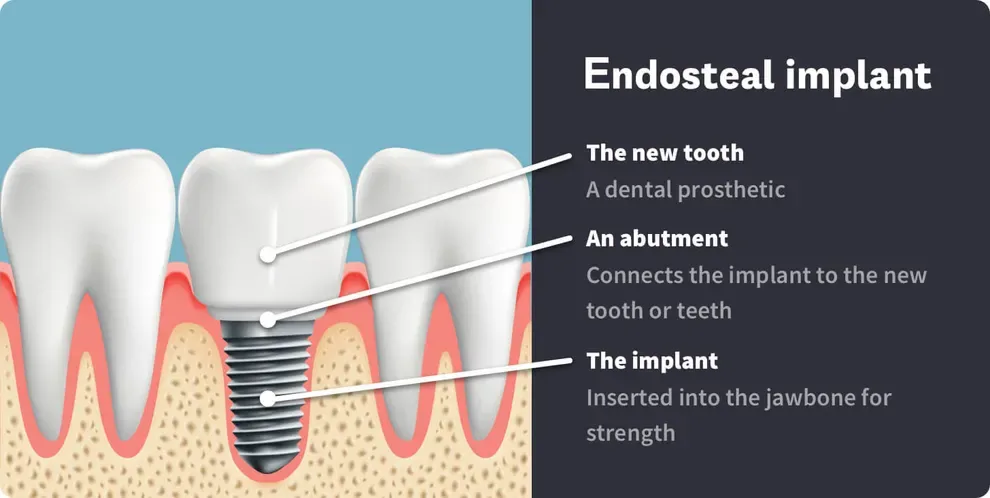
An endosteal implant, or endosseous implant, is the most commonly used dental implant and is made up of three parts:
The implant, which is inserted into the jawbone for strength
An abutment, which connects the implant to the new tooth or teeth
And the new tooth, also called a dental prosthetic
The jaw implant, abutment and the connection part of the prosthetic are made of surgical-grade titanium.
These surgical implants give dentists and oral surgeons the ability to fix problematic teeth and mouth structures with a long-term solution and deliver pain-free smiles in the process. They are an alternative to removable dentures and bridgework.
How Endosteal Implants Work
The three-piece endosteal implant creates a stronger base for new teeth, with the aim of mitigating any future issues that might result in additional crowns, bridges or root canals.
Over a period of weeks, a surgeon inserts the titanium implant base into jawbone. The newly fused bone provides support needed for talking and eating. This frame gets stronger with time, fusing with the bone, a process known as osseointegration.
After a few weeks of recovery time, an abutment gets added. The abutment is a small connector resembling a small screw that fits into the titanium implant.
The dental prosthetic, which is similar to removable dentures or fixed partial bridgework, is cemented to the abutment.
Who is a Candidate for Endosteal Implants?
An endosteal implant could be the right choice if:
You have good general health.
You have good oral health.
Your jawbone is fully developed.
You haven’t experienced any bone loss in your jaw.
You have healthy gum tissues and no periodontal diseases.
Endosteal Implant Procedure
Getting an endosteal implant happens in stages and entails multiple trips to your dentist or oral surgeon. You will have at least one consultation with your dentist about the need for an implant, followed by the creation of a replica of your jawbone(s) and the surgery itself, followed by the attachment of the abutment. Next comes the process of creating impressions for a new crown, which gets put in a couple weeks after the abutment attachment.
Last comes the addition of your new teeth. These implants can be fixed in place, or you may have the option of having removal teeth.
The implant process begins by mapping out a surgery plan with your dentist or oral surgeon.
Your dentist has to determine whether you’re a viable candidate for the endosteal implant. If necessary, the diagnosis and recommended treatment plan will be confirmed by a dental surgeon.
In these consultations, you’ll review the entire procedure and get all the information you need on the healing process and time commitments.
Endosteal implants are custom-designed, which requires an accurate replica of your jawbone. There are two ways to do this. The first is to make a cast of your jawbone. Afterward, the implant is designed on the cast and then manufactured.
The second method involves a CAT scan which is used to create a 3-D image of your jawbone. Then, a 3-D printer or milling machine is used to create a custom replica of your jawbone. Then, the implant is designed for a custom-fit.
The implant process is carried out under local or general anesthesia, so you’ll feel no pain during the process. Once numb, your surgeon will make a small incision in your gum to expose your jawbone. Next, they'll drill a hole in the bone and screw the endosteal frame deep into your bone. Your jawbone will start healing and grow into the implant.
After surgery, you’ll receive instructions for proper aftercare. You will have four to six weeks of recovery before the next phase of attaching an abutment.
You should be able to talk, drink and eat normally, with little or no discomfort, during this waiting period.
Once your surgeon is satisfied your new titanium implant has taken hold, he or she will schedule time to attach an abutment. This fastener is also made of titanium, though smaller.
Note that is some cases, the abutment is attached during the implant phase. This is something that you should plan on discussing with your surgeon as you map out the procedure and the timeline for it.
Two weeks following your abutment placement, you'll head back to your dentist’s office for impressions of your new permanent tooth (or teeth).
The final results will leave you with either fixed teeth or removal teeth. You should be able to weigh the options ahead of time on which of the two you prefer.
Fixed teeth are screwed or cemented into place and are designed to stay in place permanently, much like normal human teeth. Removal teeth snap in and out of place. You can remove them to clean them and then put them back.
Recovery and Next Steps
Like the implant process, recovery from the multiple procedures occurs in stages. Following your dentist’s care advice can help you alleviate short-term pain, long-term discomfort and provide you with a pain-free outcome—and a wonderful smile.
Immediately after you leave the dentist, you are likely to have pain and swelling. Before you swallow a pain pill on an empty stomach, use ice packs or cold packs to press against your jaw to keep the swelling down and alleviate any suffering.
You can put ice cubes into a Ziplock bag or else wrap them in a towel, using either as a compress.
You will want to stock up on soup broths, yogurt, cottage cheese and other soft foods. If you’re not already a smoothie lover, you may want to consider them as a way to make sure you’re getting enough protein.
Juicing vegetables is another way to maintain your nutrient intake without taxing your mouth.
Remember that following your procedures, you may not be able to tolerate foods that are exceptionally cold (ice cream) or hot (tea, soup).
You will also want to figure out a good regimen for constant gargling, preferably with warm salt-water or a medical saline solution, as ways to stave off infections and promote healing after each procedure.
In addition, you will want to have any over-the-counter pain medications at hand as well as any pain prescriptions you might need. Ask your dentist to write you a prescription before you receive your implant.
